
Trochanteric bursitis is a common yet often underestimated cause of hip pain that can significantly affect mobility, comfort, and overall quality of life. The condition occurs when the trochanteric bursa, a small fluid-filled sac that cushions the outer portion of the hip near the greater trochanter, becomes inflamed. This inflammation frequently leads to pain along the outside of the hip, which may worsen with activities such as walking, climbing stairs, prolonged standing, or lying on the affected side. Left unaddressed, what begins as mild irritation can progress into persistent discomfort that interferes with daily routines and physical activity.
Timely evaluation by an orthopedic specialist plays a critical role in protecting long-term hip health. Hip pain is not always straightforward, and symptoms of trochanteric bursitis can closely resemble other orthopedic conditions, such as hip arthritis, tendon injuries, labral tears, or even pain originating from the lower back. An accurate diagnosis ensures that treatment targets the true source of pain, rather than merely masking symptoms, which helps prevent chronic inflammation, muscle weakness, and recurring flare-ups. Early orthopedic care also allows for conservative treatments to be most effective, often reducing the need for more invasive interventions.
For patients in Buford, GA, access to specialized orthopedic care means hip pain does not have to become a permanent limitation. Whether discomfort is affecting work, exercise, sleep, or recreational activities around the community, recognizing when to seek professional evaluation is an important step toward recovery. Understanding the signs of trochanteric bursitis and knowing when to consult an orthopedic doctor in Buford, GA can make a meaningful difference in restoring comfort, movement, and confidence in everyday life.
If you are experiencing persistent outer-hip pain, nighttime discomfort, difficulty walking or climbing stairs, or recurring flare-ups, it is time to consult an orthopedic specialist. At Academy Orthopedics, our board-certified physicians provide thorough evaluations and personalized treatment plans for trochanteric bursitis and other hip conditions.
With nearly four decades of experience serving the Northeast Georgia community, we offer care at our Buford, Cumming, and Duluth, GA clinics, as well as at Northside Forsyth and Duluth Hospitals. Our team is dedicated to accurate diagnosis, effective treatment, and restoring mobility so you can return to your daily activities and enjoy a pain-free lifestyle.
Don’t wait for hip pain to worsen. Contact Academy Orthopedics today at 770-271-9857 or schedule a consultation online to take the first step toward relief and long-term hip health.
Understanding Trochanteric Bursitis
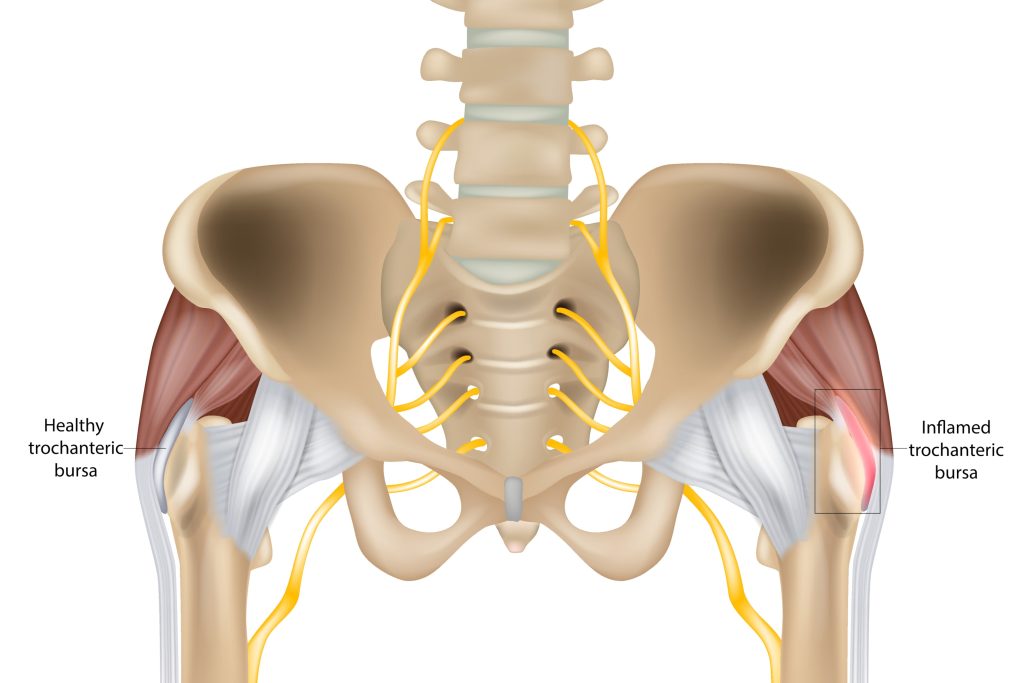
The trochanteric bursa is located over the greater trochanter of the femur, or thigh bone, which is the prominent bony area on the outer portion of the hip. Its function is to reduce friction between the bone and surrounding soft tissues, including tendons and the iliotibial band, during everyday hip movement.
When this bursa becomes inflamed, a condition commonly referred to as trochanteric bursitis and often included under the broader diagnosis of greater trochanteric pain syndrome (GTPS), irritation develops along the outside of the hip. This inflammation is typically aggravated by movement and direct pressure.
Hip bursitis can also involve other bursae within the hip region, such as the iliopsoas bursa located near the front of the hip and groin. Iliopsoas bursitis more commonly presents as groin pain, helping distinguish it from lateral hip conditions.
Common Causes
Inflammation of the trochanteric bursa may develop due to a combination of biomechanical stress and external factors, including:
- Repetitive loading from walking or running, particularly on hard or uneven surfaces
- Prolonged pressure from side-sleeping, especially on firm mattresses
- Direct trauma, such as falls or impact to the outer hip
- Leg-length differences that alter normal gait mechanics
- Tightness of the iliotibial band causing friction over the greater trochanter
- Degenerative changes in the hip or lumbar spine
- Prior hip injuries or surgical procedures
Symptoms to Recognize
Patients with trochanteric bursitis often report:
- Localized aching or sharp pain along the outer hip
- Tenderness directly over the bony prominence
- Worsening pain when lying on the affected side
- Stiffness after extended periods of sitting
- Discomfort when climbing stairs or rising from a seated position
- Increased pain with prolonged standing or walking
A key distinguishing feature is that pain typically does not originate in the groin, which helps differentiate this condition from problems within the hip joint itself. Trochanteric bursitis symptoms may extend down the outer thigh toward the knee, following the course of the iliotibial band rather than radiating into the groin or inner thigh.
👉Also Read: Managing Common Orthopedic Injuries in Cumming: Symptoms, Causes, and Treatment Solutions
Early Warning Signs That It’s Time to See an Orthopedic Doctor
Determining when hip pain requires evaluation by an orthopedic specialist is essential to preventing prolonged symptoms and functional decline. The following signs indicate that a professional assessment is warranted.
Pain lasting longer than 7 to 14 days
Outer hip pain that persists despite rest, ice, activity modification, and over-the-counter anti-inflammatory medications suggests that inflammation is not resolving on its own. Trochanteric bursitis can persist for weeks or become chronic without appropriate treatment, and early orthopedic intervention can reduce symptom duration and prevent recurrence.
Pain interfering with daily activities
Difficulty walking moderate distances, climbing stairs, or maintaining normal exercise routines indicates a loss of hip function. When hip discomfort begins to limit work responsibilities, mobility, or routine activities, further evaluation is needed to identify the source and guide targeted treatment.
Nighttime pain that disrupts sleep
Pain that prevents side sleeping or causes frequent nighttime awakenings is a common and clinically significant feature of greater trochanteric pain syndrome. Persistent night pain reflects ongoing soft tissue irritation and rarely resolves without directed care.
Visible swelling, warmth, or redness
Localized swelling, increased warmth, or skin redness over the outer hip may indicate significant inflammation and, in rare cases, infection. These findings should be evaluated promptly through a physical examination and, if necessary, diagnostic imaging or laboratory testing.
Recurrent flare-ups despite temporary improvement
Hip pain that repeatedly returns after brief periods of relief suggests unresolved biomechanical or structural contributors. Recurrent symptoms often require a comprehensive treatment plan that addresses contributing factors such as gait mechanics, muscle imbalance, or tendon involvement.
Risk Factors That Increase the Need for Orthopedic Evaluation
Certain patients should consider seeking orthopedic evaluation earlier, as specific risk factors increase the likelihood of persistent symptoms, delayed recovery, or associated tendon involvement.
Age-related changes
Hip bursitis and greater trochanteric pain syndrome occur more frequently in middle-aged and older adults, particularly women between the ages of 40 and 70. Age-related degenerative changes may include gluteus medius or minimus tendinopathy, tendon thickening, or partial tearing near the greater trochanter. These conditions often require more targeted treatment than rest alone.
History of hip injury or surgery
Patients with a history of hip replacement, fracture fixation, or arthroscopic procedures should have new onset lateral hip pain evaluated promptly. Prior surgery can alter hip biomechanics and soft tissue balance, increasing susceptibility to recurrent inflammation or tendon irritation near surgical sites or implants.
High-impact or repetitive activities
Activities that place repeated stress on the lateral hip, such as running, prolonged walking, tennis, pickleball, cycling, or physically demanding occupations involving frequent climbing or squatting, can aggravate the trochanteric region. Active individuals who experience ongoing pain should seek evaluation before continued activity leads to worsening inflammation or tendon injury.
Obesity or excess body weight
Increased body weight places greater mechanical load on the hip and surrounding soft tissues, which can reduce the effectiveness of home-based measures. Orthopedic evaluation allows for a comprehensive treatment approach that considers load management, activity modification, and supportive therapies.
Underlying medical conditions
Systemic or musculoskeletal conditions such as rheumatoid arthritis, other inflammatory arthritides, gout, lumbar spine disorders, diabetes, or leg length discrepancies can contribute to prolonged or recurrent symptoms. When these factors are present, early orthopedic involvement is especially important to ensure accurate diagnosis and coordinated care.
How an Orthopedic Doctor in Buford Diagnoses Trochanteric Bursitis
Accurate diagnosis is essential to ensure effective treatment, prevent prolonged discomfort, and avoid unnecessary rest or ineffective therapies. During your evaluation, an orthopedic doctor in Buford typically follows a structured approach.
Patient history review
Your physician will discuss the onset, duration, and character of your hip pain, as well as your daily activities, exercise habits, prior injuries or surgeries, and previous treatments. Information about medications, sleep disturbances, and associated back or groin pain helps distinguish trochanteric bursitis from other conditions such as lumbar spine disorders or intra-articular hip pathology.
Physical examination
The doctor will palpate the outer hip to assess tenderness, swelling, and warmth over the greater trochanter. Hip range of motion, muscle strength, and gait mechanics are evaluated to identify functional limitations and detect compensatory movement patterns.
Clinical tests
Specialized maneuvers assist in confirming trochanteric bursitis. Pain when lying on the affected side, discomfort with resisted hip abduction, and the Patrick-FABER test (flexion, abduction, external rotation) are commonly used. A straight leg raise or other spine assessments may also be performed to rule out referred pain from the lumbar region.
X-rays
Plain radiographs, often obtained in-office or at a local imaging center, help rule out fractures, arthritis, bone spurs, or calcifications that may irritate the bursa or contribute to lateral hip pain.
Advanced imaging
For persistent, complex, or atypical cases, MRI or musculoskeletal ultrasound may be recommended. MRI is particularly effective at detecting gluteus medius or minimus tendon tears, tendinopathy, or fluid accumulation in the hip bursa, allowing for precise treatment planning tailored to the patient’s condition.
Trochanteric Bursitis Treatment Options Offered by Orthopedic Specialists
Most patients improve with non-surgical care when treated early. Treatment plans are tailored to your activity level, overall health, and severity of symptoms.
Conservative Care
| Treatment | Purpose |
| Rest from aggravating activities | Reduces irritation of the bursa and allows inflammation to subside |
| Ice packs (10–15 minutes, several times per day) | Decreases swelling and alleviates pain |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Reduces pain and inflammation systemically |
| Topical or oral anti-inflammatory medications | Can provide pain relief comparable to corticosteroid injections in some cases |
| Physical therapy | Strengthens hip and core muscles, stretches the iliotibial band, and improves gait mechanics to prevent recurrence |
Physical therapists are integral to recovery, guiding patients through targeted strengthening and stretching exercises for the gluteus medius, hip rotators, and iliotibial band. When combined with activity modification, these interventions often lead to significant improvement or full resolution of symptoms in most patients. Therapy also addresses movement patterns that contribute to recurring irritation, reducing the risk of future flare-ups.
Activity Modification and Education
Simple adjustments to daily routines can relieve stress on the trochanteric bursa and support recovery:
- Avoid running on sloped or uneven roads
- Limit prolonged standing on hard surfaces such as concrete
- Use pillows between the knees when side-sleeping to reduce pressure on the affected hip
- Modify workstations for sitting or standing jobs to maintain neutral hip alignment
Interventional Treatments
For patients who do not achieve sufficient relief with conservative measures, several minimally invasive options may be considered:
- Corticosteroid injections: Ultrasound-guided injections into the trochanteric bursa can provide rapid pain relief, with studies showing symptom improvement in up to 90% of patients. These are most effective when combined with physical therapy.
- Platelet-rich plasma (PRP) injections: PRP therapy may be offered for chronic tendon involvement. Benefits, costs, and supporting evidence should be discussed with an orthopedic specialist.
- Extracorporeal shockwave therapy (ESWT): When paired with exercise, ESWT has demonstrated success rates around 86% at two months in some studies, occasionally outperforming steroid injections alone.
Surgical Options
Surgery is rarely required for trochanteric bursitis. Procedures such as bursectomy, iliotibial band release, or removal of damaged tissue are reserved for cases that fail several months of properly performed conservative care. Arthroscopic techniques, when indicated, allow same-day discharge and faster recovery.
Early evaluation and specialist-guided treatment can significantly reduce pain, restore function, and help patients return more quickly to walking, work, recreational activities, and restful sleep.
Choosing the Right Orthopedic Specialist in Buford, GA
Selecting an orthopedic provider experienced in hip conditions can significantly influence recovery and long-term outcomes. Specialists familiar with trochanteric bursitis, gluteal tendinopathy, and other lateral hip disorders are more likely to provide accurate diagnoses and effective, tailored treatment plans.
Credentials matter
Seek board-certified orthopedic surgeons or sports medicine specialists with documented experience in managing hip pain and greater trochanteric pain syndrome. Verified training and clinical expertise help ensure safe, evidence-based care.
Research local options
Review practice websites, provider biographies, and patient testimonials in Buford. Confirm that the specialist offers a full spectrum of care, including nonsurgical and minimally invasive treatments, rather than focusing solely on surgical intervention.
Practical considerations
Evaluate office location, availability of on-site imaging, and appointment scheduling that accommodates work and daily commitments. Convenient access can improve adherence to follow-up care and rehabilitation plans.
Comprehensive approach
An effective orthopedic specialist provides a thorough evaluation, a clear diagnosis, and a personalized treatment plan. This may combine guided home exercises, targeted injections when indicated, and scheduled follow-ups to monitor progress and reduce the risk of recurrent trochanteric bursitis.
Prevention and Long-Term Management
Once symptoms of trochanteric bursitis improve, the focus shifts to preventing recurrence and maintaining hip health. Strategies recommended by orthopedic specialists include:
Home exercise program
Physical therapists guide patients through targeted strengthening and stretching exercises to support the hip and surrounding muscles. Effective exercises often include side-lying leg lifts, clamshells, bridges, and stretches for the iliotibial band and piriformis. These routines reduce inflammation, improve hip stability, and help prevent future flare-ups.
Supportive footwear
Wearing cushioned, supportive shoes is important, particularly for prolonged walking, standing on hard surfaces, or outdoor activity. Regularly replacing worn shoes helps maintain proper biomechanics and reduces stress on the hip.
Ergonomic adjustments
Modify workstations and daily routines to reduce repetitive strain. For standing jobs, use cushioned mats and practice proper posture. For desk work, ensure chairs, desks, and monitors promote neutral hip and spine alignment.
Weight management
Maintaining a healthy weight, or achieving modest weight loss when appropriate, reduces mechanical load on the hip and lowers the risk of recurrent bursitis. Orthopedic specialists can provide guidance on safe, sustainable approaches to weight management.
Gradual activity progression
Increase exercise intensity, running, or walking distance slowly, typically no more than 10 percent per week. Vary surfaces, incorporate rest days, and pay attention to early signs of discomfort. Repetitive motion on the same surface or at high intensity can exacerbate symptoms.
Other strategies may include ongoing stretching, periodic check-ins with an orthopedic provider to assess the bursa and surrounding structures, and individualized modifications to physical activity based on recovery and response to treatment.
👉Also Read: Hip Arthritis And You
Expert Care for Hip Pain Starts at Academy Orthopedics in Buford
Trochanteric bursitis is a common and treatable cause of outer-hip pain, but if left untreated, it can become a chronic problem that limits mobility and daily activities. Early evaluation and treatment are key, and most patients experience relief within weeks with the right care.
If you are experiencing hip pain lasting more than one to two weeks, nighttime discomfort, difficulty walking or climbing stairs, or recurring flare-ups, it is time to consult a specialist.
At Academy Orthopedics in Buford, GA, our orthopedic team provides precise diagnosis and customized treatment plans for trochanteric bursitis and other lateral hip conditions. From targeted injections to minimally invasive procedures, we focus on relieving pain, restoring function, and preventing recurrence.
Don’t let hip pain limit your life. Schedule a consultation with Academy Orthopedics today and take the first step toward long-lasting relief, improved mobility, and a more active, comfortable lifestyle.
Frequently Asked Questions
How do you treat trochanteric bursitis?
The best treatment depends on symptom severity, but most cases improve with conservative care. This includes activity modification, anti-inflammatory medications, ice, and avoiding positions that aggravate the outer hip. If pain persists, ultrasound-guided corticosteroid injections can provide effective relief. Surgery is rarely needed and is reserved for cases that do not respond to nonsurgical treatment.
Can I still exercise if I have hip bursitis, or should I stop all activity?
Complete rest is rarely necessary and may actually slow recovery. However, you should avoid high-impact activities or movements that cause pain directly over the hip. Lower-impact exercises are typically safe and beneficial during recovery, including easy cycling, swimming, pool walking, or using an elliptical machine.
How long does it usually take to feel better after starting treatment with an orthopedic doctor?
Recovery timelines vary depending on symptom severity and duration. Some patients notice improvement within 2 to 4 weeks when treated with anti-inflammatory medications such as NSAIDs and activity modifications. Chronic cases, especially those involving underlying tendinopathy, may take 2 to 3 months or longer to fully resolve. Consistency with activity adjustments and adherence to your orthopedic doctor’s recommendations significantly affect recovery speed.
Is trochanteric bursitis the same as hip arthritis?
No. Trochanteric bursitis involves inflammation of the bursa and surrounding soft tissues on the outer hip, causing lateral pain that worsens with side-lying or walking. Hip arthritis affects the joint surfaces themselves and usually causes groin pain, stiffness, and difficulty with movements such as putting on shoes, socks, or getting in and out of a car. An orthopedic doctor can distinguish between these conditions through a combination of physical examination and imaging studies.
Will a cortisone injection cure my trochanteric bursitis symptoms permanently?
Corticosteroid injections can provide strong short- to medium-term pain relief, but they are most effective when paired with strategies to address underlying causes, such as activity modification and targeted strengthening. A single injection will not permanently correct biomechanical issues or muscle weakness. Repeated injections are used cautiously, as long-term steroid use can affect tendon health. Surgery or other interventions are considered only if conservative treatments fail.
