
Is your shoulder silently freezing up, making simple tasks like brushing your hair or reaching for a shelf feel like a painful challenge? You’re not alone. Frozen shoulder, or adhesive capsulitis, is a surprisingly common yet misunderstood condition that can turn everyday movement into a source of frustration. But here’s the good news: understanding what’s happening beneath the surface is the first step toward reclaiming your mobility. In this guide, we unravel the mystery behind frozen shoulder—what causes it, how to recognize the signs, and the latest treatments to help you thaw the stiffness and get back to living pain-free.
Key Takeaways
- Frozen shoulder, or adhesive capsulitis, leads to pain and restriction of shoulder movement, significantly affecting daily activities and quality of life.
- Key causes include inflammation, scar tissue formation, underlying health conditions like diabetes, and prolonged immobility, with symptoms worsening over time.
- Frozen shoulder treatment focuses on pain management and restoring mobility through physical therapy, medications, and potentially surgical options, with recovery typically taking up to two years.
If you’re experiencing persistent shoulder stiffness or pain that interferes with your daily activities, it’s time to take the next step toward lasting relief. At Academy Orthopedics, our board-certified orthopedic surgeons specialize in diagnosing and treating frozen shoulder with both non-surgical therapies and advanced surgical options like capsular release and shoulder arthroscopy.
With nearly four decades of orthopedic excellence, we deliver personalized care plans designed to restore your mobility and improve your quality of life. Don’t let frozen shoulder hold you back—schedule a consultation at one of our convenient Georgia locations in Cumming, Buford, or Duluth. Call (770) 271-9857 or book your appointment online and begin your path to recovery with a trusted orthopedic team.
👉Also Read: The Hidden Signs of a Labrum Shoulder Tear: How to Spot a SLAP Tear Early
Understanding Frozen Shoulder
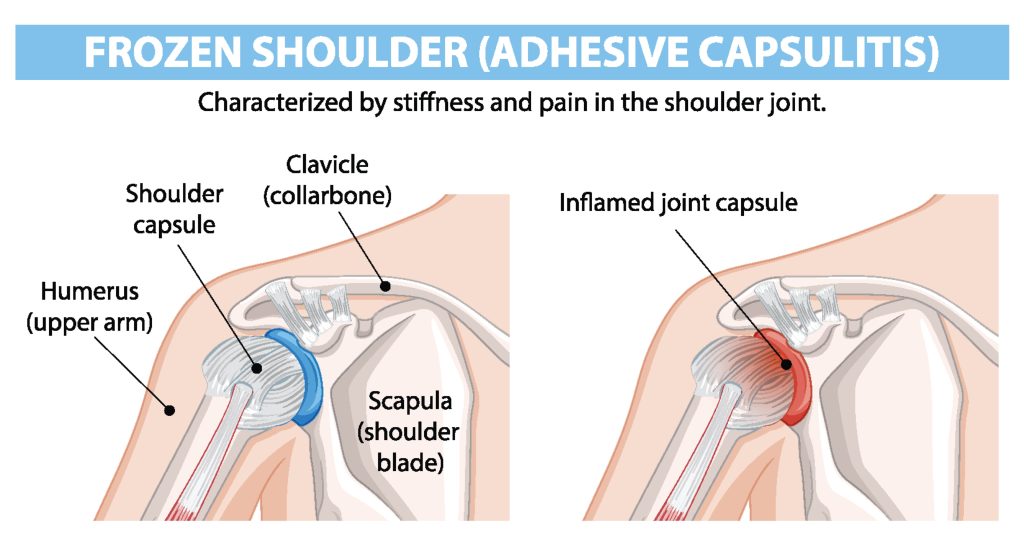
Frozen shoulder, medically called adhesive capsulitis, is a progressive condition characterized by pain, stiffness, and a substantial decrease in the shoulder joint’s range of motion. It typically develops gradually and can severely impact daily activities, diminishing overall quality of life.
What Is Frozen Shoulder?
Frozen shoulder develops when the connective tissue around the shoulder joint—the joint capsule—becomes thickened and tight, limiting movement and causing ongoing pain. Over time, this limitation increases, leading to stiffness and difficulty performing even routine tasks such as reaching, lifting, or dressing.
Diagnosis is based on a comprehensive review of the patient’s medical history, clinical symptoms, and physical examination. Imaging tests, such as X-rays or ultrasound, may be used to rule out other shoulder conditions, such as rotator cuff tears or arthritis.
Anatomy and Mechanism of Frozen Shoulder (Adhesive Capsulitis)
The shoulder joint capsule is a fibrous structure that envelops the joint, providing stability. In frozen shoulder, this capsule becomes inflamed, thickened, and develops adhesions—bands of stiff connective tissue—that limit the movement of the soft tissues surrounding the joint.
Additionally, there is often a reduction in synovial fluid, the natural lubricant of the joint, which further contributes to restricted mobility and discomfort.
The rotator cuff, a group of muscles and tendons responsible for shoulder stability and motion, may also be affected indirectly due to compensatory movement patterns or inflammation in the joint area.
Clarifying Common Misconceptions About Frozen Shoulder
Despite its prevalence, frozen shoulder is often misunderstood. Several common misconceptions can lead to delayed diagnosis or inappropriate treatment:
- It only affects older adults: While frozen shoulder is more common in individuals between the ages of 40 and 60, it can also occur in younger individuals, particularly those recovering from shoulder injuries or surgeries, or with underlying health conditions such as diabetes.
- It is the same as a rotator cuff injury: Though both conditions affect shoulder movement, they differ significantly. Frozen shoulder involves the thickening and tightening of the joint capsule, while rotator cuff injuries involve damage to the muscles or tendons surrounding the joint.
- It goes away quickly on its own: Frozen shoulder progresses in stages—freezing, frozen, and thawing—often taking months or even years to resolve fully. Without appropriate management, symptoms may persist or worsen.
- Movement worsens the condition: While certain movements may cause discomfort during flare-ups, gentle, guided physical therapy is essential for recovery. Prolonged immobilization can actually exacerbate stiffness and delay improvement.
- Surgery is always required: Most cases of frozen shoulder can be managed non-surgically through a combination of physical therapy, anti-inflammatory medications, and sometimes corticosteroid injections. Surgery is typically reserved for severe or unresponsive cases.
Causes of Frozen Shoulder
Understanding the causes of frozen shoulder is crucial for both prevention and timely management. The condition typically arises from a combination of biological and mechanical factors that lead to the progressive stiffening of the shoulder joint.
Primary Mechanisms
The hallmark of frozen shoulder is inflammation of the shoulder joint capsule, which initiates a cascade of physiological changes. Over time, this inflammation promotes the development of fibrotic tissue and adhesions—bands of scar-like tissue that bind the joint and limit movement. Concurrent thickening and contracture of the shoulder capsule further contribute to restricted mobility and chronic pain.
Contributing Medical Conditions
Several underlying health conditions are strongly associated with the development of frozen shoulder, including:
- Diabetes mellitus: Individuals with diabetes are at significantly higher risk, up to five times more likely, due to altered collagen metabolism and increased systemic inflammation.
- Thyroid disorders: Both hyperthyroidism and hypothyroidism are linked to increased incidence, possibly due to hormonal imbalances affecting connective tissues.
- Parkinson’s disease and cardiovascular conditions: These systemic illnesses may also predispose individuals by limiting movement and contributing to inflammatory responses.
Post-Immobilization Onset
Frozen shoulder can also develop following periods of shoulder immobility, often due to:
- Post-operative recovery (e.g., rotator cuff repair or mastectomy)
- Fractures or dislocations requiring immobilization
- Stroke, which may cause prolonged inactivity on one side of the body
Immobility can allow inflammation to set in and restrict normal joint movement, hastening the onset of adhesive capsulitis.
Risk Factors
Certain demographic and lifestyle factors elevate the risk of developing frozen shoulder:
- Age: Most commonly affects adults between 40 and 60 years
- Gender: Women are disproportionately affected
- Previous shoulder injuries: Trauma or repetitive strain can initiate inflammation
- Sedentary lifestyle: Limited physical activity may impair joint health and recovery
- Surgical history: Particularly involving the chest, breast, or shoulder region
Frozen Shoulder Symptoms
Frozen shoulder typically unfolds in three distinct stages: freezing, frozen, and thawing. Each stage presents a unique pattern of symptoms and can last for several months, making early recognition and management essential. The primary features include progressive shoulder pain and restricted range of motion, both of which can significantly impair daily functioning.
Stage 1: Freezing Stage (Lasts 6 to 12 Weeks)
This initial phase is characterized by a gradual onset of shoulder pain that worsens over time:
- Pain with movement becomes more prominent and often disrupts sleep.
- Stiffness begins to develop, making overhead and backward movements increasingly difficult.
- Daily tasks such as reaching for objects or dressing become uncomfortable.
During this stage, pain is the dominant symptom, and mobility gradually starts to decline.
Stage 2: Frozen Stage (Lasts 4 to 6 Months)
As inflammation subsides, the shoulder becomes increasingly stiff:
- Pain may decrease, particularly at rest.
- Severe restriction of movement persists, especially in external rotation and abduction.
- Functional limitations become more pronounced, making tasks like grooming, driving, or lifting nearly impossible without assistance.
At this point, stiffness is the most disabling feature, though pain may still occur with movement.
Stage 3: Thawing Stage (Lasts 6 Months to 2 Years)
In the final stage, shoulder mobility gradually begins to improve:
- Range of motion slowly returns, although full recovery may take time.
- Pain continues to diminish, often resolving entirely by the end of this stage.
- Residual stiffness may linger, but usually responds well to consistent physical therapy and home exercise.
The thawing stage can be prolonged, and full recovery varies based on factors such as age, underlying health conditions, and adherence to treatment.
Diagnosing Frozen Shoulder
Frozen shoulder is primarily diagnosed through a detailed clinical evaluation, often supplemented by imaging to confirm findings and exclude other conditions. Early diagnosis helps guide timely and effective treatment.
Medical History and Physical Examination
The diagnostic process begins with a thorough review of the patient’s symptoms and medical history. During the physical examination, the physician assesses both active and passive range of motion, focusing on movements such as external rotation and abduction.
A key clinical sign is a significant and persistent loss of shoulder mobility, especially when both the patient and the examiner are unable to move the joint through its normal range. The examination may also include checks for tenderness and an evaluation of posture to identify contributing factors from surrounding structures, such as the neck or upper back.
Imaging Tests
While frozen shoulder is often diagnosed clinically, imaging studies are used to exclude other conditions such as arthritis, rotator cuff tears, or calcific tendonitis.
- X-rays help rule out bone abnormalities or joint degeneration.
- MRI can reveal thickening of the joint capsule and inflammation consistent with adhesive capsulitis.
- Ultrasound is occasionally used to assess soft tissue structures and joint capsule integrity.
Advanced imaging supports the diagnosis and ensures that alternative causes of shoulder pain are accurately excluded.
👉Also Read: The Ultimate Guide to Sports Medicine: Enhancing Athletic Performance and Recovery
Treatment Options for Frozen Shoulder
Managing frozen shoulder (adhesive capsulitis) involves a comprehensive approach focused on alleviating pain, restoring shoulder mobility, and rebuilding strength. The primary objective of treatment is to reduce inflammation and prevent further stiffness in the joint, allowing for a gradual return to daily activities.
Treatment options typically begin with non-surgical methods, such as pain relief medications and physical therapy, which aim to improve flexibility and function. In more severe cases, additional interventions may be considered to provide further relief and support recovery.
Non-Surgical Treatments
Non-surgical management remains the primary approach for treating frozen shoulder, particularly in its early and moderate stages. The goal is to reduce pain, restore mobility, and improve function through a combination of physical therapy, medications, and conservative interventions.
Physical therapy plays a central role, with a focus on targeted range-of-motion and stretching exercises designed to gradually restore joint flexibility. These exercises should be performed consistently under the guidance of a licensed physical therapist. To prepare the shoulder for activity, patients are often advised to apply moist heat, such as a warm shower, bath, or heating pad, for 10 to 15 minutes beforehand. This helps to relax the muscles and ease stiffness, making movement less painful.
Patients are strongly encouraged to avoid overhead reaching, heavy lifting, or any activities that exacerbate shoulder pain during the treatment period. Alternative therapies, such as acupuncture, may also offer pain relief for some individuals, although these should be viewed as complementary to a structured physical rehabilitation program.
Medications and Injections
Pain management is another critical component of non-surgical treatment. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, are commonly used to reduce inflammation and alleviate discomfort. In more severe cases, corticosteroid injections may be administered directly into the joint to control inflammation and facilitate mobility. Another effective intervention is hydrodilatation, in which a saline solution—often combined with a steroid—is injected into the joint capsule to gently stretch the tissue and relieve tension.
Surgical Interventions
In cases where symptoms persist despite months of conservative treatment, additional non-surgical procedures may be considered. One option is manipulation under anesthesia, where the shoulder is gently moved through its range of motion while the patient is sedated, to break up adhesions. Another is capsular distension, in which fluid is injected into the joint to further expand and loosen the capsule.
Surgery is rarely necessary, but in severe, unresponsive cases, arthroscopic capsular release may be performed. This minimally invasive procedure involves removing thickened scar tissue from the shoulder joint to restore mobility. Most patients, however, respond well to non-surgical care and can expect significant improvement over time with a dedicated and consistent treatment plan.
Recovery and Prevention
The recovery from frozen shoulder typically unfolds over a period of 12 to 36 months and progresses through three distinct phases: freezing, frozen, and thawing. Each stage has its own timeline and symptom profile. The freezing phase, which lasts from 6 weeks to 9 months, is marked by increasing pain and a gradual loss of motion. The frozen phase can extend from 4 to 12 months and is characterized by reduced pain but significant stiffness and limited mobility. The final thawing phase may last from 6 months to 2 years, during which shoulder motion gradually improves, often returning close to normal with consistent therapy.
Preventive Measures
Preventing frozen shoulder involves maintaining regular shoulder movement and addressing risk factors early. One of the most effective strategies is to keep the shoulder joint active, especially after injury, surgery, or any period of immobilization. Patients recovering from a stroke, mastectomy, or rotator cuff injury should engage in gentle range-of-motion exercises as recommended by their healthcare provider to prevent stiffness.
Managing underlying health conditions such as diabetes, thyroid disorders, and cardiovascular disease is also essential, as these are known risk factors for adhesive capsulitis. Practicing good posture, avoiding repetitive strain, and incorporating daily stretching routines can further reduce the risk. For individuals with a history of frozen shoulder, continuing a guided physical therapy program even after recovery may help prevent recurrence and promote long-term joint health.
👉Also Read: Choosing the Right Specialist: What Doctor Should I See for Shoulder Pain?
Reclaim Your Shoulder Mobility with Academy Orthopedics Today!
Living with frozen shoulder can feel like a constant negotiation with your own body—each movement a reminder of limitation. At Academy Orthopedics, we understand that no two shoulders—and no two patients—are the same. That’s why we offer personalized, evidence-based care designed to restore motion, reduce pain, and help you regain control of your daily life. Whether you are in the early stages of stiffness or seeking alternatives after months of limited mobility, our orthopedic specialists are here to guide you with clarity, compassion, and clinical precision. Don’t let frozen shoulder dictate your quality of life—reach out to Academy Orthopedics today and take your first confident step toward recovery.
