
A fractured tibia, known as a broken shinbone, is one of the most serious lower leg injuries and a commonly fractured long bone due to its critical role in bearing weight and supporting movement. These fractures often result from high-impact trauma, sports injuries, or sudden falls. As the primary weight-bearing bone of the lower limb, the tibia is essential for mobility and overall stability. When injured, it can lead to intense pain, swelling, and difficulty walking or bearing weight, making early recognition and timely medical care vital for optimal recovery.
In this guide, we’ll explore the telltale symptoms of a tibial fracture, discuss why diagnosis isn’t always straightforward, and explain when to seek medical attention. We’ll also highlight how early, expert care can prevent complications and accelerate recovery. At Academy Orthopedics, we’re committed to helping you move from pain to progress with compassionate, personalized orthopedic treatment designed to restore your strength and mobility.
What Are the Key Symptoms of a Fractured Tibia?
Identifying the signs of a fractured tibia and fibula early is critical for receiving appropriate and timely care. While some symptoms are immediate and pronounced, others may develop gradually, especially in cases involving stress fractures or hairline breaks. Understanding the hallmark indicators can help patients—and those caring for them—recognize when professional orthopedic evaluation is necessary.
Localized Swelling and Bruising
One of the earliest and most visible signs of a tibial fracture is severe pain and swelling around the shin area. This swelling is often accompanied by bruising due to blood vessel damage near the fracture site. The area may become warm and tender to the touch, and the skin might appear discolored as bleeding occurs under the surface. Persistent or worsening swelling should never be ignored, as it may signal internal complications such as compartment syndrome.
Inability to Bear Weight or Walk
Difficulty standing or walking is a strong indicator of a structural injury to the tibia. Patients often describe a sudden onset of weakness or instability in the leg. In more severe tibial shaft fractures, any attempt to bear weight can be extremely painful or physically impossible. If walking is impaired following a fall, direct blow, or accident, immediate orthopedic assessment is advised.
Visible Deformity or Bone Protrusion (in Severe Cases)
In cases of compound or displaced fractures, the leg may appear visibly deformed. This may present as a twisted or angulated appearance, and in extreme scenarios, bone may protrude through the skin. These are medical emergencies requiring urgent surgical intervention to prevent infection, nerve damage, or vascular compromise.
Deep, Aching Pain Not Relieved by Rest
Unlike muscular soreness or minor bruises, a tibial fracture typically produces a deep, constant pain that does not subside with rest, elevation, or over-the-counter medications. The pain may worsen with movement or pressure, and patients often describe it as a sharp, throbbing, or intense ache that signals an underlying break in the bone structure.
Numbness or Tingling from Nerve Involvement
In some cases, particularly when swelling compresses nearby nerves, patients may experience numbness, tingling, or a “pins and needles” sensation in the foot or lower leg. This symptom indicates possible nerve involvement and requires prompt evaluation to prevent long-term neurological damage.
Why Recognizing a Tibia Fracture Isn’t Always Straightforward
While some tibial fractures present with unmistakable symptoms, others may be deceptively subtle, leading to delays in diagnosis and proper care. Several factors can obscure the severity of the injury, particularly in the early stages. Misinterpretation of symptoms, individual pain thresholds, and the temptation to self-diagnose often contribute to missed or delayed treatment, increasing the risk of complications.
Common Misconceptions: “It’s Just a Sprain”
One of the most frequent errors individuals make is assuming that their symptoms are consistent with a mild sprain or contusion, especially in the absence of a visible deformity or open wound. Minor swelling, bruising, and discomfort are often attributed to overuse or a benign injury. Unfortunately, this mindset can lead patients to underestimate the seriousness of their condition. Unlike soft tissue injuries, fractures require specific stabilization and often imaging to confirm the extent of damage. Mislabeling a tibia or fibula fracture as a sprain can result in prolonged pain, improper healing, and long-term mobility issues.
The Role of Pain Tolerance and Delayed Symptom Escalation
Pain perception varies greatly between individuals. Those with a high tolerance for discomfort may continue to walk or engage in daily activities despite having a fracture. In cases of stress or hairline fractures, symptoms may begin as a dull ache and only intensify over time. This gradual escalation can make it difficult for patients to recognize the need for medical intervention until the damage has worsened. In athletes or active individuals, this is particularly dangerous, as continued weight-bearing can transform a small fracture into a complete break.
Risks of Misdiagnosis or Self-Treatment
Attempting to manage a suspected injury at home—using rest, ice, compression, and elevation (RICE), for instance—may provide temporary relief but can obscure the underlying structural damage. Without proper imaging and evaluation, fractures can be missed, leading to improper healing or complications such as nonunion (where the bone fails to heal) or malunion (where it heals incorrectly). Additionally, misdiagnosed tibial fractures may continue to bear stress from daily movement, increasing the risk of more serious injury, chronic pain, and future orthopedic intervention.
Acute vs. Gradual Symptoms: How Tibia Fracture Presentations Can Vary
Not all tibia fractures present the same way. While some occur suddenly and unmistakably, others develop gradually, with symptoms that may be easily overlooked until the damage progresses.
High-Impact vs. Stress Fracture Symptoms
Acute tibial fractures often result from high-energy trauma such as a car accident, sports collision, or a significant fall. These injuries typically present with immediate and intense symptoms—sharp pain, swelling, bruising, and an inability to bear weight. In more severe cases, there may be visible bone deformity or skin puncture from an open fracture, prompting urgent medical attention.
In contrast, stress fractures of the tibia develop from repetitive strain, often in athletes, runners, or individuals engaged in high-impact physical activity over time. These microfractures usually begin with a dull, localized pain that worsens with activity and may initially subside with rest. Because symptoms evolve gradually, they are frequently mistaken for shin splints or muscle fatigue, delaying diagnosis and treatment.
Gradual Onset in Athletes or Active Individuals
Among athletes and active individuals, the subtle onset of pain can be misleading. It may begin as a mild discomfort during or after exercise and increase in intensity as training continues. Without intervention, what starts as a stress response in the bone can progress into a full fracture. Timely evaluation, especially when pain becomes persistent despite rest, is crucial to avoid complications.
Differences in Pediatric and Adult Presentations
Age also plays a significant role in how tibia fractures present. In children, bones are still developing and may bend or crack rather than break completely, leading to what’s known as a greenstick or buckle fracture. These injuries may cause less obvious deformities but still require medical evaluation and stabilization. Adults, especially older individuals with lower bone density, are more susceptible to complete fractures from seemingly minor falls or impacts, often with more pronounced symptoms and longer recovery periods.
Differentiating a Chipped Tibia from Severe Fractures
Not all tibia fractures present with the same severity. A chipped tibia (avulsion fracture) typically involves a small bone fragment breaking away from the main shaft and often causes less intense symptoms than a full or complex fracture. However, even minor injuries—such as stress fractures or small chips—should not be overlooked, as they can lead to significant complications if left untreated.
Severe fractures may involve multiple fragments (comminuted fractures) or a diagonal break across the bone (oblique fractures), often requiring surgical intervention. Accurately distinguishing between different fracture types is critical for determining the most effective treatment plan and preventing further injury. Prompt diagnosis and appropriate management can prevent minor injuries from progressing into more serious, long-term issues.
When to Seek Emergency Care vs. Orthopedic Evaluation
A tibia fracture is a serious injury that can range in severity, from stress-related microfractures to full-thickness breaks involving surrounding nerves, blood vessels, or skin. Knowing when to seek immediate emergency care versus scheduling an orthopedic evaluation is critical to ensuring the injury is managed safely and effectively.
Signs Requiring Immediate Emergency Room Care
Certain symptoms signal a medical emergency and require a prompt visit to the ER. These include:
- An obvious bone deformity or visible bone protrusion through the skin
- Severe swelling, bruising, or bleeding at the injury site
- Inability to move the leg or complete inability to bear weight
- Numbness, tingling, or loss of sensation in the foot or lower leg (suggesting nerve involvement)
- Pale, cool, or blue-tinted skin below the injury site (which may indicate compromised blood flow)
In these cases, delay in fractured tibia treatment could result in long-term complications such as permanent nerve damage, poor bone alignment, infection (in open fractures), or even compartment syndrome—a painful and potentially dangerous condition involving pressure buildup in muscle compartments.
Situations Appropriate for Next-Day Orthopedic Consultation
Not all tibia injuries require emergency intervention. In cases where the pain is tolerable, there’s no visible deformity, and the patient can still move the limb or bear limited weight (even if with difficulty), a next-day appointment with an orthopedic specialist is typically appropriate. These include:
- Suspected stress fractures presenting with localized pain during activity but improving with rest
- Mild to moderate swelling and tenderness without bruising or numbness
- Stable injury following initial ER evaluation or urgent care visit
Prompt orthopedic evaluation remains essential even in these less acute scenarios, as early diagnosis and appropriate management can prevent worsening of the fracture or further complications.
The Danger of “Walking It Off” or Delaying Imaging
Some individuals, particularly athletes or those with a high pain threshold, may attempt to “walk it off” or delay medical imaging under the assumption that the injury is minor. This can be a costly mistake. Continuing to bear weight on a fractured tibia—even a small stress fracture—can worsen the damage, delay healing, and increase the risk of requiring surgical intervention. Moreover, untreated fractures can heal improperly, leading to chronic pain, mobility limitations, and long-term joint instability.
How Is a Tibial Fracture Diagnosed?
When a tibial fracture is suspected, an accurate and timely diagnosis is essential for guiding treatment and preventing complications. At Academy Orthopedics, we use a combination of clinical evaluation and advanced imaging to determine the presence, location, and severity of the fracture, as well as to rule out other potential causes of lower leg pain.
The Importance of Physical Examination
The diagnostic process begins with a thorough physical examination. A skilled orthopedic provider will assess for visible deformities, localized tenderness, swelling, and any signs of instability in the leg. Functional tests—such as checking range of motion, gait, or weight-bearing ability—may also be performed. In some cases, specific areas of the tibia are palpated to isolate pain and determine whether the fracture may involve the shaft, plateau, or distal end.
Neurological and vascular assessments are also essential, especially when symptoms include numbness, tingling, or discoloration of the foot. These findings may indicate nerve or vessel involvement, which could significantly impact treatment urgency and prognosis.
Imaging: X-Ray, CT Scan, or MRI
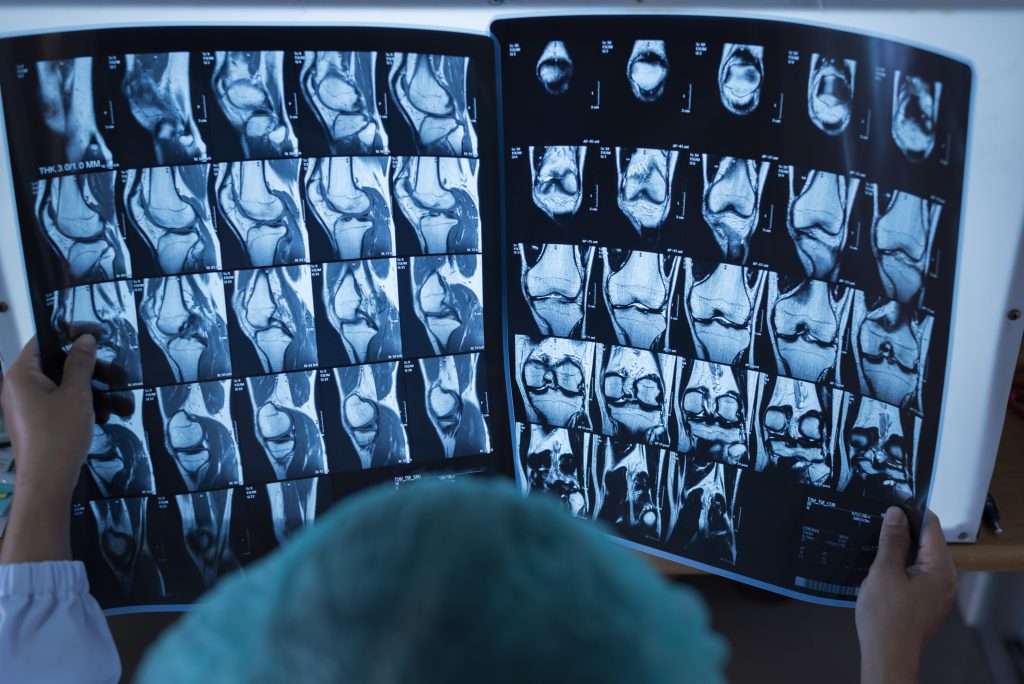
While a physical exam provides valuable initial clues, imaging is necessary to confirm a tibial fracture and understand its full extent:
- X-rays are the first-line imaging tool, offering clear visualization of bone alignment, displacement, or fragmentation. They help classify the fracture type (e.g., transverse fracture, oblique or spiral fracture) and identify whether the break is open or closed.
- CT scans provide a more detailed, three-dimensional view, particularly useful for evaluating complex or joint-involving fractures, such as tibial plateau injuries.
- MRI scans are particularly valuable for detecting stress fractures, hairline cracks, or associated soft tissue damage (including ligaments, tendons, and cartilage), which may not appear on standard X-rays.
Selecting the appropriate imaging modality depends on the mechanism of injury, the clinical presentation, and the suspected type of fracture.
Differential Diagnosis: Distinguishing from Shin Splints or Ligament Injury
Not all lower leg pain is due to a fracture, and one of the key roles of diagnostic evaluation is to rule out other conditions that mimic a tibial fracture. For example:
- Shin splints (medial tibial stress syndrome) commonly cause diffuse pain along the inner edge of the tibia, particularly in runners or athletes. Unlike fractures, this pain typically improves with rest and lacks point tenderness or swelling.
- Ligament injuries may present with instability or joint pain, but often involve the knee joint or ankle rather than the bone itself. MRI imaging is particularly useful in differentiating these soft tissue injuries from bone trauma.
By combining physical assessment with targeted imaging and a detailed clinical history, our orthopedic team ensures that patients receive a precise diagnosis and a personalized treatment plan, avoiding unnecessary interventions and promoting optimal recovery outcomes.
What to Expect at Your First Orthopedic Appointment
For individuals experiencing symptoms of a tibial fracture—whether due to a traumatic incident or ongoing pain—the first visit to an orthopedic specialist is a pivotal step in the path toward recovery. At Academy Orthopedics, our goal is to provide prompt, personalized care that prioritizes both comfort and clarity from the moment you walk through our doors.
Initial Patient Evaluation: History and Symptoms
Your appointment will begin with a comprehensive review of your medical history and a focused discussion of the events leading up to your symptoms. Whether your symptoms followed a direct trauma, developed gradually during physical activity, or appeared without an obvious cause, these details help your provider understand the potential nature of the injury.
You’ll be asked about the onset, location, and progression of your pain, any associated symptoms such as swelling, numbness, or difficulty walking, and whether you’ve attempted any home treatments. This history is essential to differentiate between fracture types—such as acute breaks versus stress fractures—and to evaluate the likelihood of associated injuries.
Timeline of Diagnostic Imaging
Based on your symptoms and physical examination, your provider will determine which imaging tests are needed and when they should be conducted. In most cases, an in-office X-ray will be performed immediately to assess for visible fractures or bone misalignment. If the X-ray is inconclusive, or if there is concern for a complex fracture, stress fracture, or soft tissue involvement, a CT scan or MRI may be ordered either the same day or within a few days.
Our team will explain each imaging modality’s purpose and what the findings may mean for your diagnosis and treatment plan.
Discussion of Stabilization, Casting, or Surgical Recommendations
Once imaging results are available, your orthopedic specialist will explain the diagnosis and recommend a course of action. Treatment options depend on the location and severity of the fracture:
- Stable, non-displaced fractures may be treated conservatively with immobilization, such as a cast or walking boot, often accompanied by activity modifications and follow-up monitoring.
- Displaced or unstable fractures might require surgical intervention to realign and stabilize the bone using internal fixation (e.g., rods, plates, or screws).
- Stress fractures may be managed with rest, bracing, physical therapy, and gradual return to activity.
Throughout this process, our team ensures you understand every step of your care. You’ll be informed of the expected healing timeline, potential complications, and what to expect during follow-up appointments. Whether your treatment plan involves surgery, physical therapy, or conservative management, we’re here to guide you through it with skill and compassion.
Schedule a Personalized Evaluation at Academy Orthopedics
If you suspect a fractured tibia, broken bone, or are experiencing persistent leg pain, don’t wait to seek answers. At Academy Orthopedics, we understand how critical early diagnosis and targeted treatment are to your recovery and long-term mobility. Our team is committed to providing comprehensive evaluations, advanced imaging, and individualized care plans tailored to your condition and lifestyle. Whether you’re recovering from a sports injury, an accident, or unexplained pain, we’re here to guide you every step of the way.
Take control of your healing—contact Academy Orthopedics today to schedule your personalized consultation.
Frequently Asked Questions
Do all tibia fractures require surgery?
Not all tibia fractures require surgical intervention. The need for surgery largely depends on the type, location, and severity of the fracture, as well as the patient’s overall health and activity level.
How long does it take to recover from a tibia fracture?
Recovery time from a tibia fracture can vary significantly depending on the severity of the break, the type of treatment received, and individual factors such as age, overall health, and activity level. In general, most uncomplicated tibia fractures take between 3 to 6 months to heal, though full recovery—including regaining strength, mobility, and function—may extend beyond this period.
For non-surgical cases managed with immobilization, healing may begin within a few weeks, but weight-bearing activities are typically restricted until there is clear evidence of bone healing on imaging.
What is the fastest way to heal a broken tibia?
The fastest way to heal a broken tibia is to seek prompt medical care and follow your orthopedic provider’s treatment plan closely. Proper immobilization, a nutrient-rich diet, and avoiding smoking or alcohol can significantly support bone healing. Physical therapy, when advised, also helps restore strength and speed up recovery.
